The Soaring Use of SSRI Anti-depressants in the United States
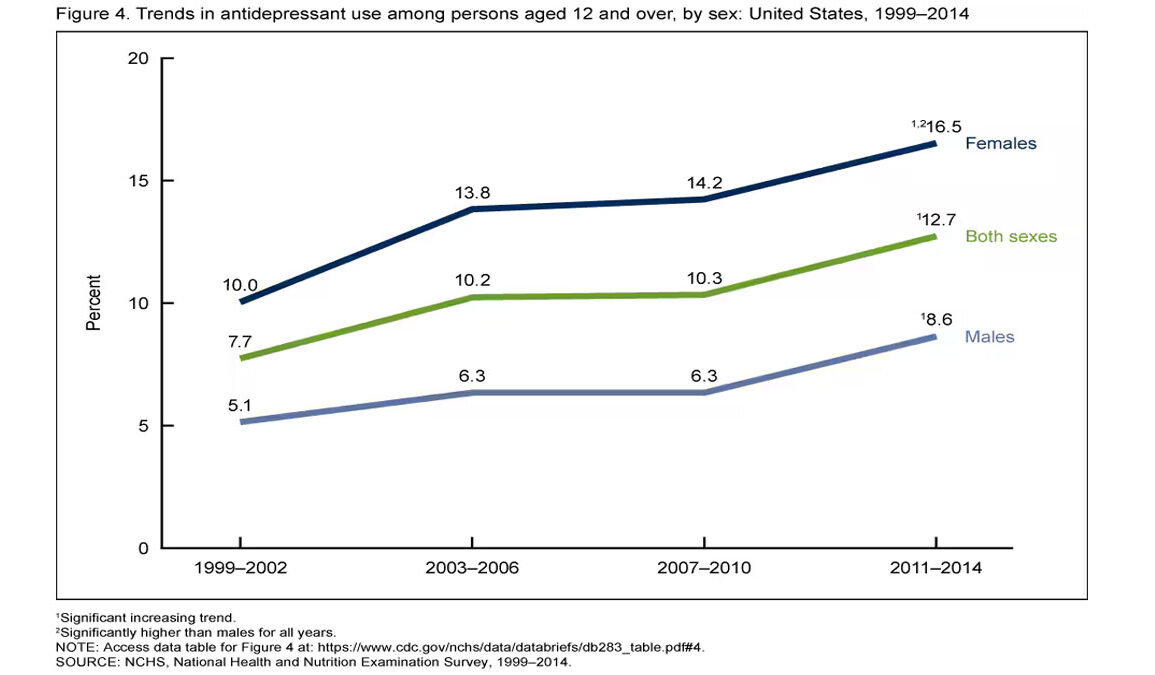
In the past two decades, the use of antidepressants in America has increased dramatically. According to the Centers for Disease Control and Prevention (CDC), nearly 17% of American adults take prescription medication for depression or anxiety. Women are prescribed these medications at nearly twice the rate of men. Among young adults, the numbers are even more striking, particularly in cities like Seattle.
What Are SSRIs and How Do They Work?
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed medications for treating depression and anxiety disorders in the United States. These drugs, including well-known brands like Prozac (fluoxetine), Zoloft (sertraline), Celexa (citalopram), and Lexapro (escitalopram), function by increasing serotonin levels in the brain. Serotonin is a neurotransmitter associated with mood regulation, and SSRIs work by preventing its reabsorption, theoretically making more of it available to help stabilize emotions.
The widespread use of SSRIs has led to an ongoing debate regarding their effectiveness, safety, and potential overprescription. Some studies suggest they can significantly improve symptoms for those with clinical depression and anxiety disorders, but other research questions whether they are significantly more effective than placebos in mild to moderate cases. This has raised concerns about whether SSRIs are being prescribed too readily, especially when non-medication-based therapies such as cognitive behavioral therapy (CBT) might be viable alternatives.
How Addictive Are SSRIs?
One of the key controversies surrounding SSRIs is whether they are addictive. While they do not produce the same type of chemical dependency seen with opioids or benzodiazepines, they can lead to what is known as “SSRI discontinuation syndrome.”
Symptoms of SSRI withdrawal can be severe and include dizziness, nausea, irritability, fatigue, and what some describe as “brain zaps”—unpleasant electrical shock-like sensations in the brain. Some patients experience withdrawal symptoms that last for weeks or even months. This has led some experts to argue that, while not classified as addictive, SSRIs can create a form of dependence that makes discontinuing them difficult.
Robert F. Kennedy Jr., who is leading a federal effort to scrutinize the use of SSRIs, has called them “highly addictive, potentially dangerous and overprescribed.” These concerns align with a growing sentiment among healthcare professionals and policymakers that SSRIs may be used excessively without thorough consideration of long-term effects or alternative treatments.
Seattle: A Case Study in Antidepressant Use
New research suggests that the use of SSRIs and other antidepressants is particularly high in Seattle, raising concerns about the extent to which these medications are being relied upon. According to data from Nielsen surveys:
- 33% of women aged 18-35 in Seattle—an estimated 205,000 individuals—reported using medication for depression or anxiety in the past year.
- In contrast, only 15% of men in the same age range—about 102,000 individuals—reported similar usage.
- Among all adults in the Seattle metro area, 19% reported using these medications, slightly above the national average of 17%.
This data places Seattle among the top U.S. cities for antidepressant and anti-anxiety medication use, ranking seventh in the country for the share of young women taking these medications. The rates are even higher in cities like Salt Lake City (41%) and Boston (36%), while cities in the Sunbelt, including San Antonio, Dallas, and Los Angeles, report significantly lower rates between 10% and 15%.
Why Are Women Using These Medications at Higher Rates Than Men?
The significant gender gap in SSRI usage raises important questions. Nationally, 23.5% of young women use medication to treat depression or anxiety, compared to 14% of young men. While depression and anxiety do appear to be more common in women, experts also point to societal and medical biases that may lead to overprescription among female patients.
Research suggests that women are more likely to seek medical help for emotional distress and are often prescribed medication as the first line of treatment, whereas men are more likely to have their symptoms dismissed or be encouraged to seek alternative treatments such as exercise or behavioral therapy.
RFK Jr. and Trump’s Commission: A Challenge to the Status Quo
In response to these concerning trends, former President Donald Trump has issued an executive order establishing the “Make America Healthy Again” Commission, appointing Robert F. Kennedy Jr. as its head. The commission has been tasked with assessing the “prevalence and threat” of SSRIs and similar drugs.
Kennedy, known for his skepticism of pharmaceutical companies, has been vocal about what he sees as the overuse of psychiatric medications. He has argued that SSRIs have been handed out too freely, often without proper oversight or exploration of alternative therapies.
“The increase in prescriptions for these drugs is alarming,” Kennedy stated. “We need to carefully examine the long-term consequences of medicating an entire generation.”
The commission’s creation has sparked fierce debate. Mental health advocates worry that reducing access to these medications could harm those who genuinely need them. However, critics of the pharmaceutical industry argue that the push for SSRIs has led to a culture where medication is seen as the first, and sometimes only, solution for emotional distress.
The Bigger Picture: Why This Matters
The increasing reliance on SSRIs, especially among young adults, raises several troubling questions:
- Are we over-medicating mental health conditions?
- Why are women being prescribed at such disproportionately high rates?
- What are the long-term effects of widespread SSRI use on public health?
- Are alternative treatments being sidelined in favor of pharmaceutical solutions?
Some experts argue that our mental health crisis is symptomatic of deeper societal problems, including economic instability, social isolation, and a lack of access to holistic mental health care. Instead of simply increasing prescriptions, they advocate for a more comprehensive approach to mental well-being, including greater access to therapy, community support programs, and lifestyle interventions.
As the debate intensifies, one thing is clear: America’s dependence on SSRIs is reaching unprecedented levels. The findings from Seattle provide a stark reminder that while medication can be beneficial, it should not be the sole response to a complex mental health crisis. A broader discussion on mental health care, societal stressors, and responsible prescribing practices is long overdue.