What Is Sepsis?
Sepsis is a life-threatening medical condition that occurs when the body’s immune system overreacts to an infection, triggering widespread inflammation that can lead to organ failure, tissue damage, and death. Instead of fighting the infection, the immune system turns against the body, causing a cascade of harmful effects.
Sepsis can develop from any infection, but it is most commonly caused by bacterial infections such as pneumonia, urinary tract infections, or abdominal infections. Viral and fungal infections, including COVID-19 and the flu, can also lead to sepsis.
How Deadly Is Sepsis? The Alarming Statistics
Sepsis is one of the leading causes of death worldwide. According to the World Health Organization (WHO), in 2020, there were an estimated 49 million cases of sepsis globally and 11 million deaths, accounting for 20% of all deaths worldwide. In the United States alone, the Centers for Disease Control and Prevention (CDC) reports that 1.7 million people develop sepsis each year, with nearly 350,000 deaths annually.
Children under five, the elderly, and those with weakened immune systems are at the highest risk. Alarmingly, nearly 20 million cases of sepsis occur in children under five every year. Despite these staggering numbers, sepsis remains under-recognized, leading to delayed treatment and preventable deaths.
The Stages of Sepsis
Sepsis progresses rapidly and can escalate within hours. It is categorized into three stages:
- Sepsis – The body responds abnormally to an infection, causing inflammation that spreads through the bloodstream.
- Severe Sepsis – The infection leads to organ dysfunction, affecting critical functions like kidney filtration and oxygen exchange.
- Septic Shock – Blood pressure drops to dangerously low levels, causing multiple organ failure, respiratory distress, heart failure, and death if not treated immediately.
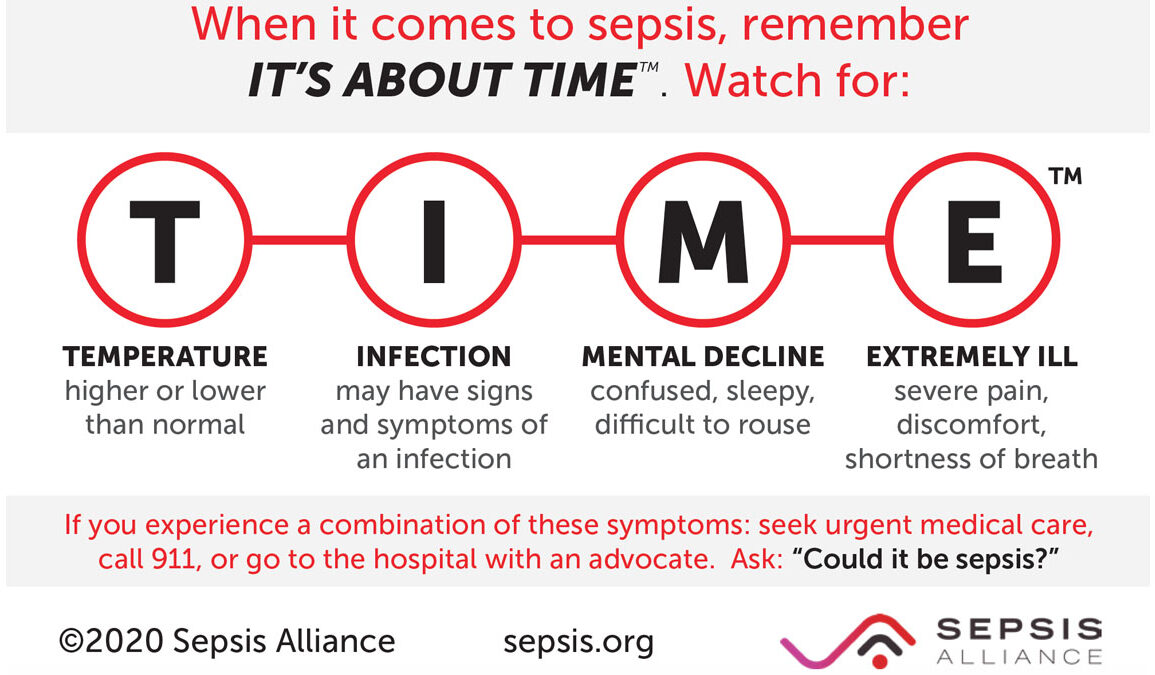
Recognizing the Symptoms of Sepsis
Early detection is critical, as each hour without treatment increases the risk of death by up to 9%. The symptoms of sepsis can be mistaken for other conditions like pneumonia or the flu, making it essential to recognize the warning signs:
- Fever or abnormally low temperature
- Chills and shivering
- Rapid heart rate
- Shortness of breath
- Confusion or disorientation
- Extreme pain or discomfort
- Sweaty, clammy, or pale skin
- Low blood pressure
In severe cases, sepsis may cause blue discoloration of the lips or extremities, decreased urination, and difficulty waking up.
Who Is Most at Risk for Sepsis?
While sepsis can affect anyone, certain individuals face a higher risk, including:
- Newborns and infants
- Adults over 65 years old
- People with weakened immune systems (e.g., cancer patients, HIV/AIDS patients, transplant recipients)
- Individuals with chronic conditions such as diabetes, kidney disease, or liver disease
- Hospitalized patients, particularly those in intensive care units (ICUs)
- People with invasive medical devices, such as catheters or ventilators
What To Do If You Suspect Sepsis
Sepsis is a medical emergency. If you or someone you know exhibits symptoms of sepsis, seek immediate medical attention. Prompt treatment dramatically improves survival rates.
Diagnosing and Treating Sepsis
Doctors diagnose sepsis based on symptoms, blood tests, and imaging scans to identify the source of the infection. Two key diagnostic criteria include:
- Systemic Inflammatory Response Syndrome (SIRS): Requires meeting at least two of the following—high or low body temperature, increased heart rate, rapid breathing, or abnormal white blood cell count.
- Quick Sequential Organ Failure Assessment (qSOFA): Evaluates low blood pressure, high respiratory rate, and altered mental status.
Treatment for sepsis often includes:
- Immediate IV antibiotics to fight the infection
- Fluids and vasopressors to maintain blood pressure
- Oxygen therapy or ventilators for breathing support
- Dialysis for kidney failure
- Surgery to remove infected tissues or drain abscesses
The Road to Recovery: Long-Term Effects of Sepsis
Surviving sepsis doesn’t mean the battle is over. Many patients experience long-term complications, known as post-sepsis syndrome (PSS). This affects up to 50% of sepsis survivors and may include:
- Fatigue and muscle weakness
- Cognitive impairment (difficulty concentrating, memory loss)
- Chronic pain and nerve damage
- Depression, anxiety, or PTSD
- Organ damage, leading to long-term kidney, liver, or heart issues
Preventing Sepsis: What You Can Do
The best way to prevent sepsis is to prevent infections and seek early treatment for any suspected infection. Key preventive measures include:
- Good hygiene – Wash hands frequently and keep wounds clean.
- Vaccinations – Stay up to date on flu, pneumonia, and other vaccines.
- Prompt treatment – See a doctor at the first sign of an infection.
- Managing chronic conditions – Keep diabetes, kidney disease, or other illnesses under control.
The Global Fight Against Sepsis
Sepsis remains a massive public health challenge, with disparities in incidence and survival rates across different regions. Low- and middle-income countries have the highest rates of sepsis, due to limited healthcare access, poor sanitation, and high infection rates.
In response to this crisis, the WHO adopted Resolution WHA70.7, which prioritizes better sepsis diagnosis, treatment, and prevention worldwide. Additionally, new research initiatives, such as Harvard’s Sepsis Epidemiology and Prevention Studies (SEPSIS) Center, aim to improve sepsis surveillance, treatment strategies, and policy measures to save lives.
The Bottom Line: Don’t Ignore Sepsis
Sepsis is a medical emergency that can escalate within hours. Recognizing the symptoms and getting immediate treatment can mean the difference between life and death. While medical advancements continue to improve outcomes, prevention remains the best defense. Stay vigilant, take infections seriously, and never ignore the warning signs of sepsis.